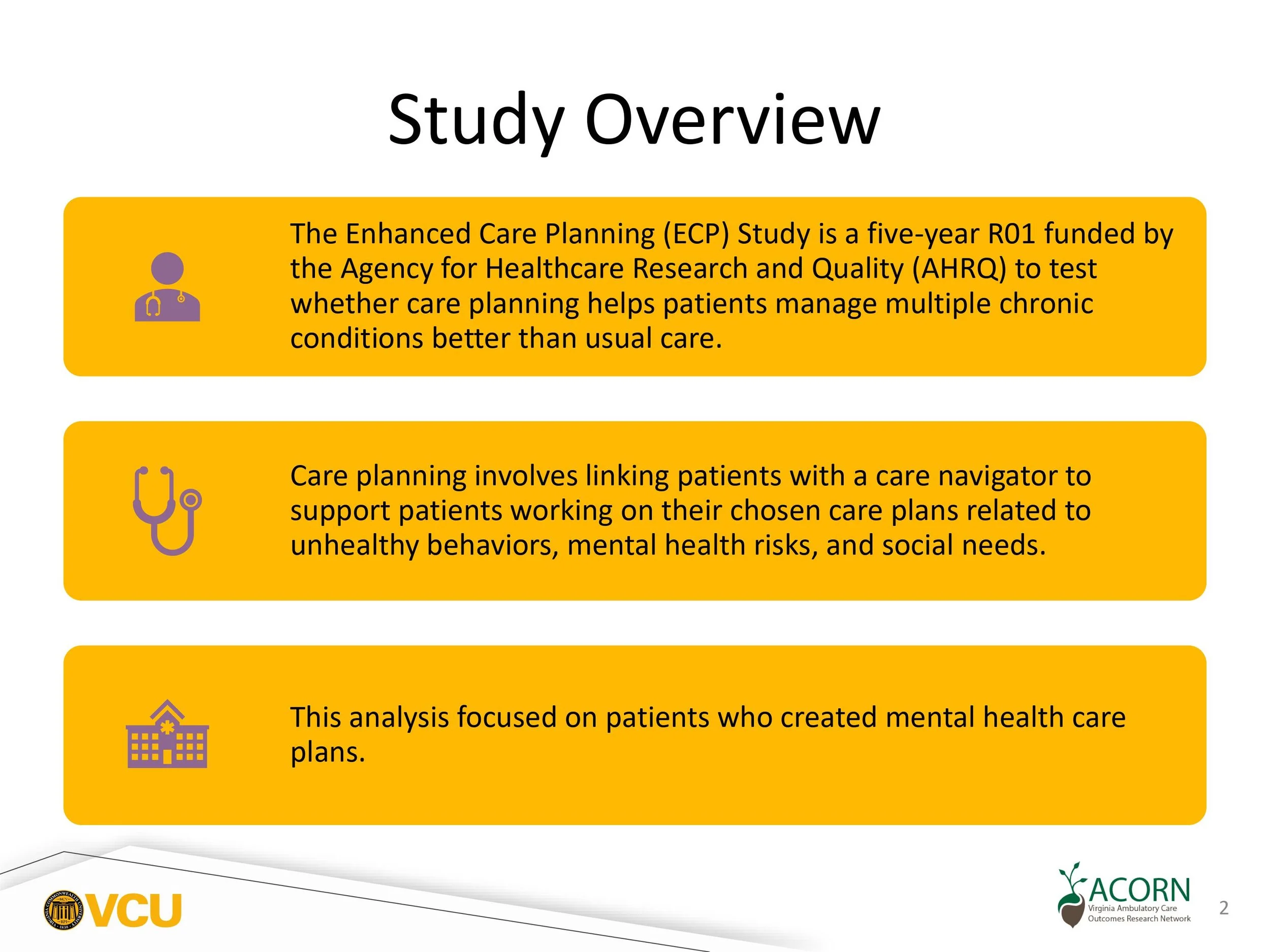
Preliminary Results and Findings
Patient Preferences for Addressing Unhealthy Behaviors, Mental Health Challenges, and Social Needs in Primary Care
Guidelines recommend addressing health behaviors, mental health, and social needs in primary care. However, it is unclear how often patients want support to address these risks. As part of a randomized trial comparing enhanced care planning versus usual care, we evaluated what risks patients wanted to address. All patients with multiple chronic conditions, 1 or more of which was uncontrolled, from 81 clinicians in 30 primary care practices. Using My Own Health Report (MOHR), patients identified and prioritized their health risks to create a care plan. All patients had at least 1 unhealthy behavior (100%) and most had a mental health risk (66.8%) and a social need (51.3%). Participants more often chose to create care plans addressing unhealthy behaviors (92.5%) rather than mental health (23.2%), or social needs (12.5%). The most frequently created care plans were for exercise (65.1%), weight loss (37.2%), and nutrition (36.2%). All patients had 1 or more unhealthy behaviors, mental health risks, or social needs, and were more likely to address health behaviors. We need to better understand these patient choices, and change the culture to normalize the integration of mental health and social care into primary care. Click on the image to read the full article.
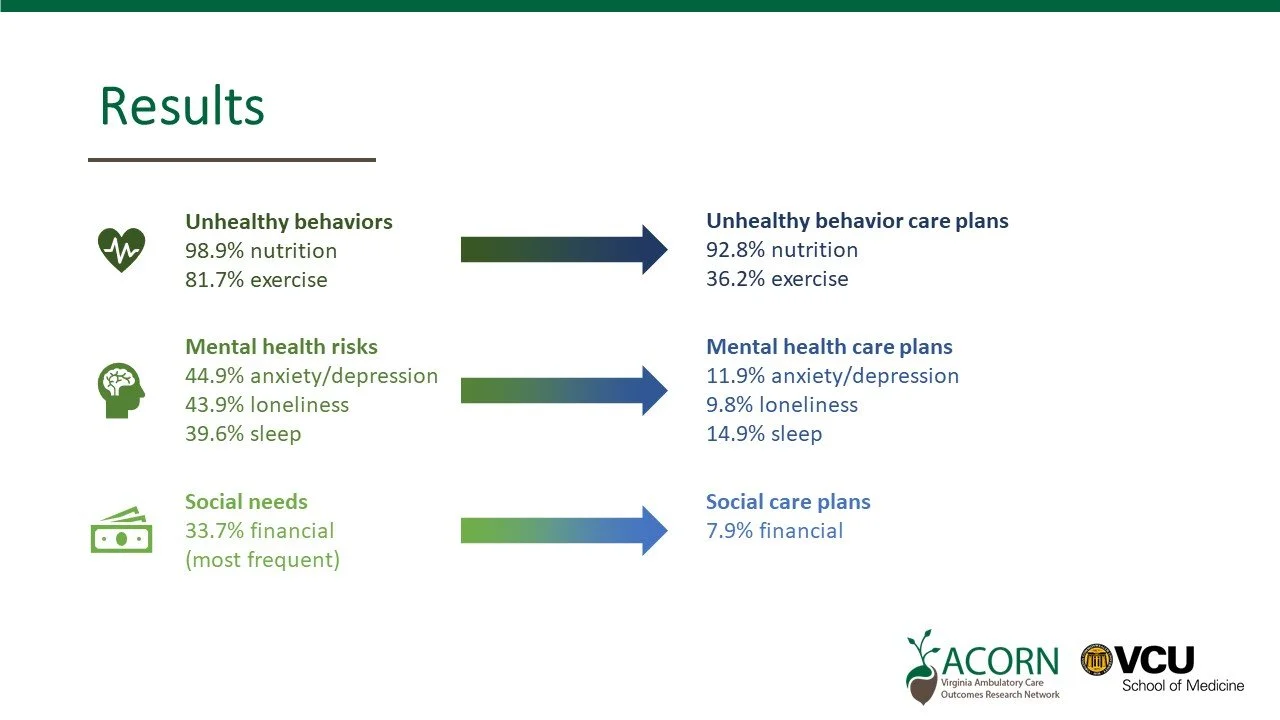
Patient preferences in addressing health needs
We looked at Health Risk Assessments and care plans created by patients with multiple chronic conditions. The majority of intervention patients had nutrition (98.9%) and exercise (81.7%) risks. For mental health, 44.9% of patients had risks for anxiety or depression, 43.9% had risks for loneliness, and 39.6% had poor sleep. For social needs, the most frequent risk was financial (33.7%). Across all health risks, patients most frequently created care plans to address unhealthy behaviors for exercise (92.8%) and nutrition (36.2%). Patients less frequently created care plans for anxiety or depression (11.9%), loneliness (9.8%), and sleep (14.9%). In primary care, the vast majority of patients have health risks in nutrition and exercise and chose to create a care plan to address these needs. Many patients also have mental health risks, but less chose to create a care plan to address them. Long term, interventions are needed to change patient interest and expectation about working with primary care teams to address mental health and social needs.
This was chosen as a plenary presentation at the Practice-Based Research Network conference in Reston, VA in June 2024!
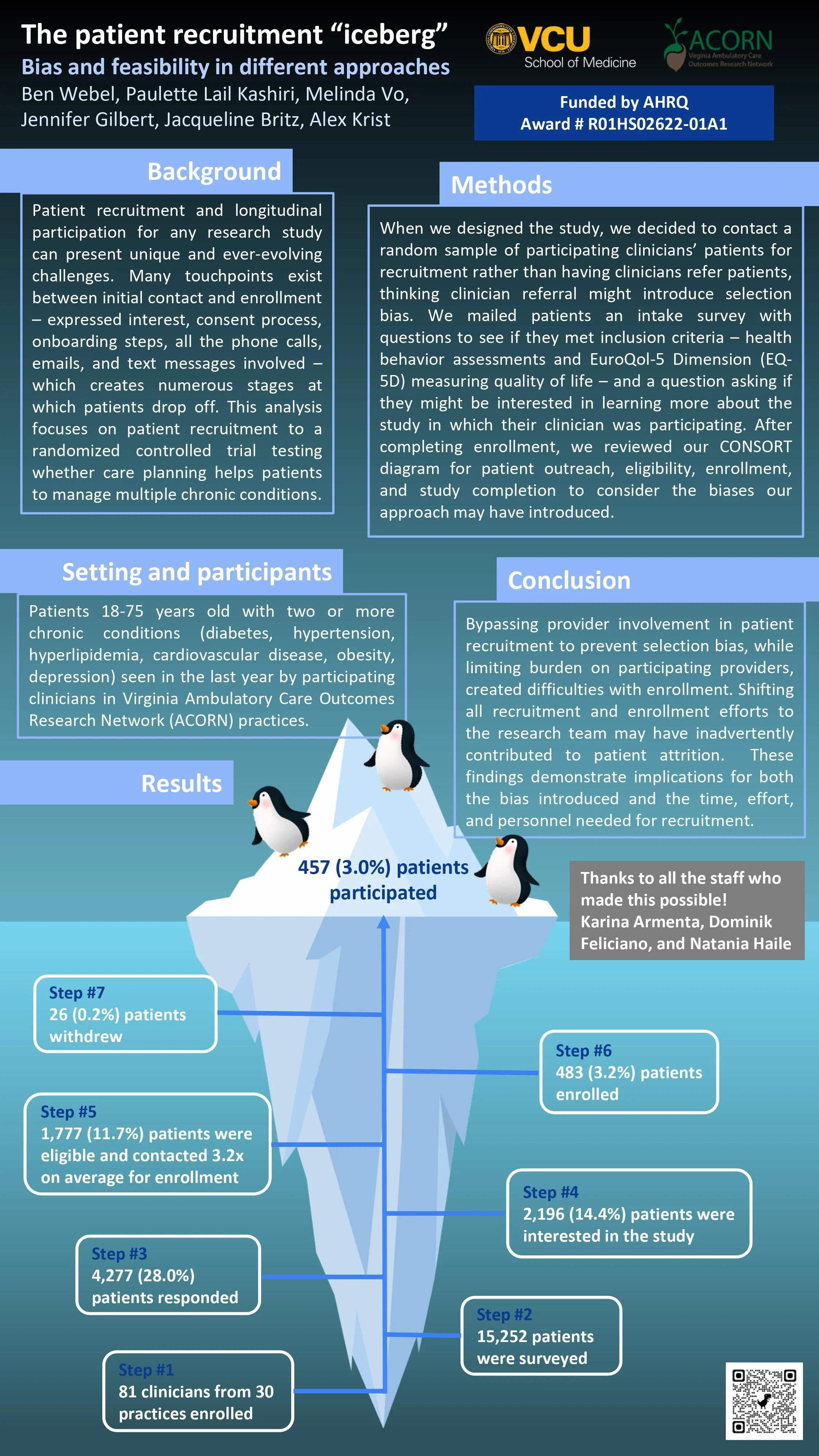
Looking at bias and feasibility in different recruitment approaches
Patient recruitment and longitudinal participation for any research study can present unique and ever-evolving challenges. When we designed this study, we decided to contact a random sample of participating clinicians’ patients for recruitment rather than having clinicians refer patients, thinking clinician referral might introduce selection bias. Bypassing provider involvement in patient recruitment to prevent selection bias, while limiting burden on participating providers, created difficulties with enrollment. Shifting all recruitment and enrollment efforts to the research team may have inadvertently contributed to patient attrition. These findings demonstrate implications for both the bias introduced and the time, effort, and personnel needed for recruitment.
We presented these results at the Practice-Based Research Network conference in Reston, VA in June 2024 and won the Outstanding Poster award!
Summer research program
Each summer, students between their first and second years of medical school join our team for four weeks. They assist with general research tasks and work closely with faculty and staff mentors to develop a research question within the project and prepare a presentation for our annual Primary Care Research Student Symposium. Many students also choose to submit their work to local and/or national conferences.
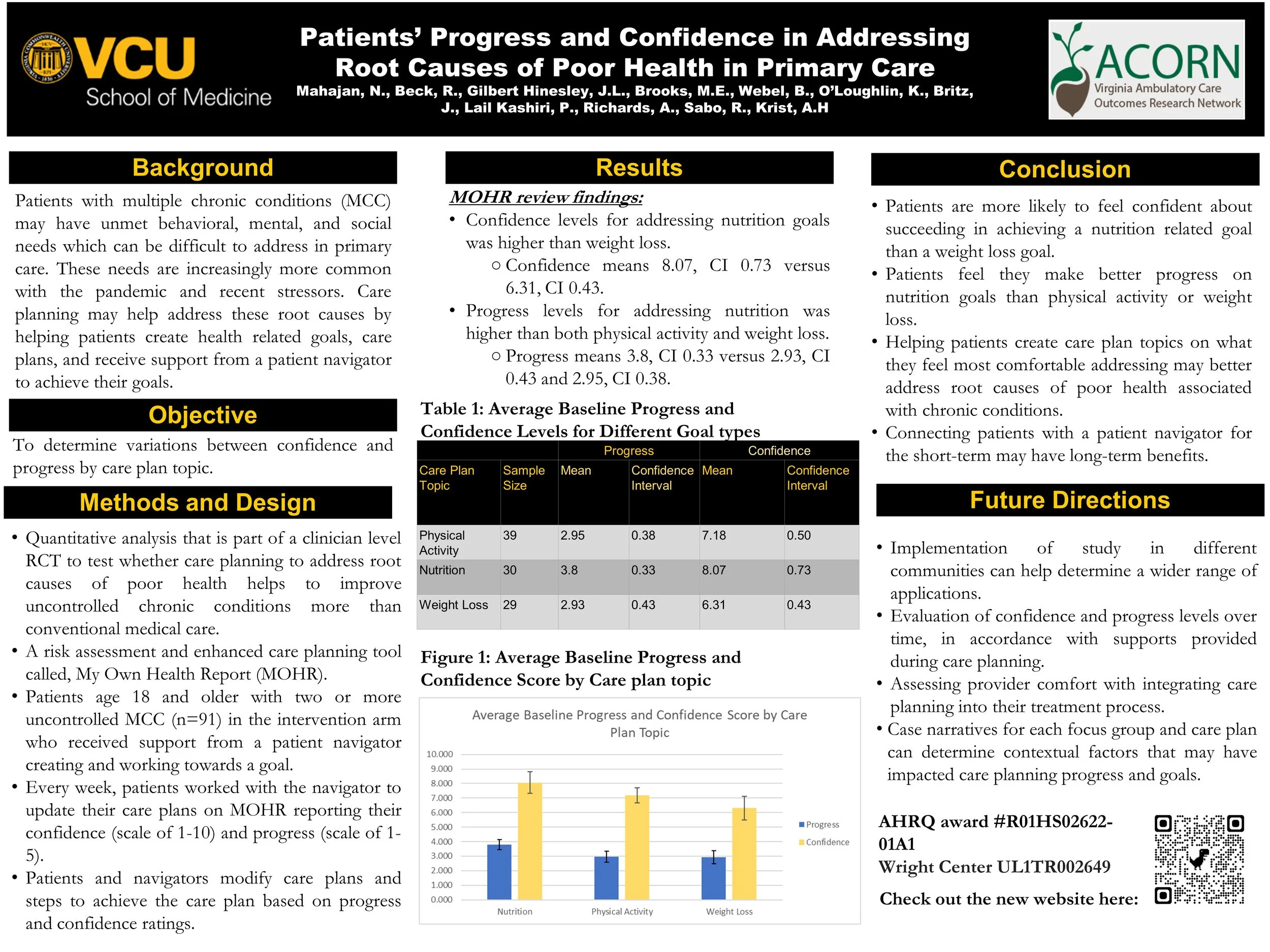
In 2022, Nihar Mahajan and Beck Regan looked at care plans created by patients enrolled in the study to determine variations between patient-reported confidence and progress by care plan topic. They found that patients are more likely to feel confident about succeeding in achieving a nutrition-related goal than a weight loss goal, and that patients feel they make better progress on nutrition goals than physical activity or weight loss. So, helping patients create care plan topics on what they feel most comfortable addressing may better address root causes of poor health associated with chronic conditions. Click the image to see the poster they presented at the North American Primary Care Research Group annual meeting, where they were PaCE approved!
In 2024, Cameron Kelly conducted an analysis for participants who made care plans to address their mental health using self-reported progress and confidence, and EQ-5D-5L index scores (standardized measure for health-related quality of life). She found that patients reported progress in meeting their mental health care goals, particularly in the sleep domain, many patients described positive quality of life benefits from participating in care planning, and patients reported higher confidence at the end of care planning for loneliness and sleep care plans, but not anxiety/depression.
In 2023, Alexis Dorsey reviewed which actions enrolled patients selected to complete their care plan goals (n=149 goals; 1,222 selected actions). She found that 66% of actions are self-directed, meaning the patient can do them at home or without a navigator connecting them, and that most patients chose less than 10 actions. Click the image to see her presentation slides.
Community referrals for patients with multiple chronic conditions
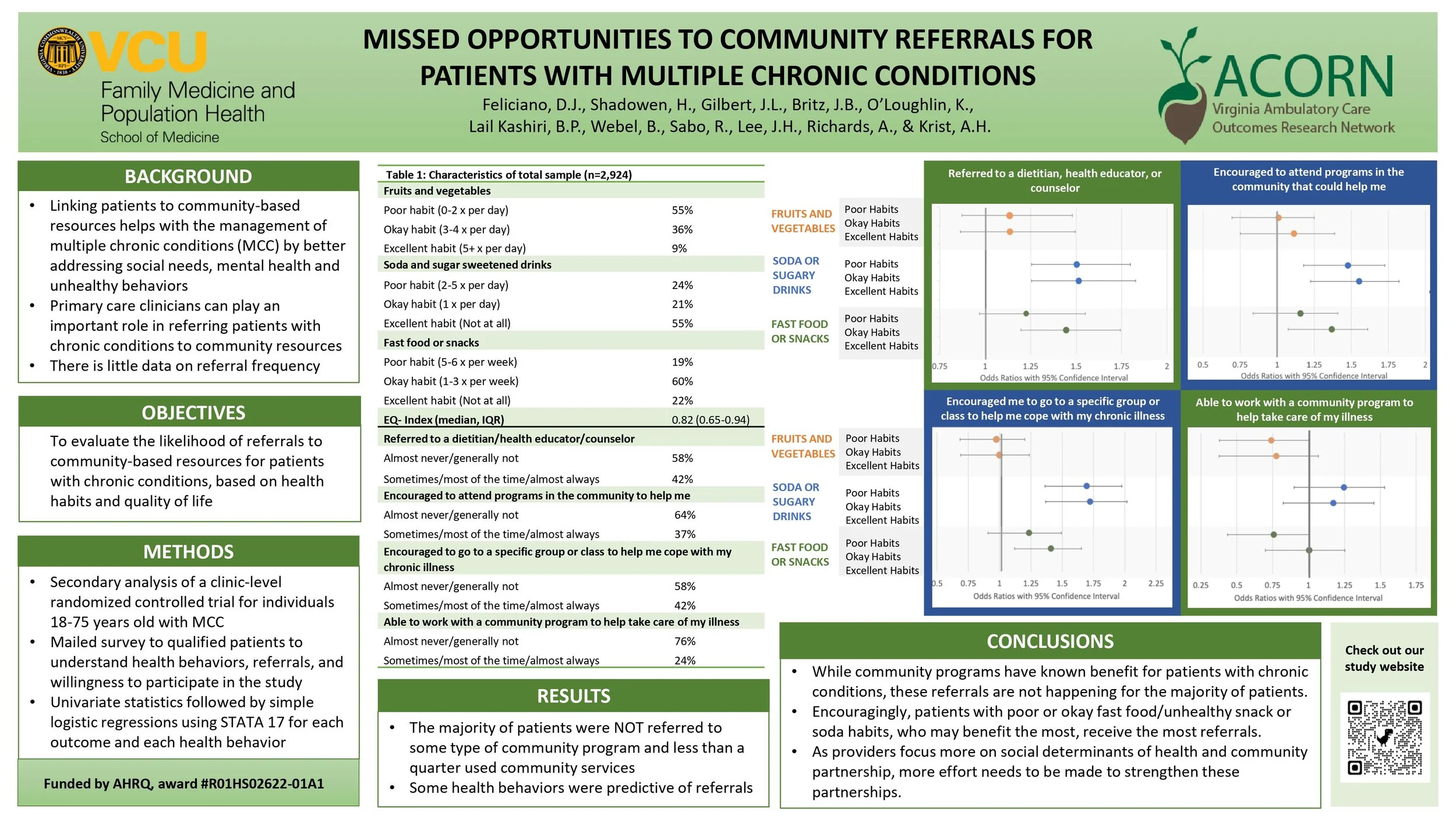
Dominik Feliciano (research assistant) and Hannah Shadowen (MD/PhD student) evaluated the likelihood of referrals to community-based resources for patients with chronic conditions, based on their self-reported health habits and quality of life. The majority of patients were NOT referred to some type of community program and less than a quarter used community services. Some health behaviors were predictive of referrals. They concluded that while community programs have known benefit for patients with chronic conditions, these referrals are not happening for the majority of patients. Encouragingly, patients with poor or okay fast food/unhealthy snack or soda habits, who may benefit the most, receive the most referrals. As providers focus more on social determinants of health and community partnership, more effort needs to be made to strengthen these partnerships. Click the image to see the poster they presented at the Practice-Based Research Network Conference in May 2023, where they were selected for the poster walk.
The feasibility of patient navigation for care planning in primary care
To help better control chronic conditions we need to address root causes of poor health like unhealthy behaviors, mental health, and social needs. However, addressing these needs in primary care is difficult. One solution may be connecting patients with a navigator for support creating a personal care goal. As part of an RCT to evaluate a feasible approach to care planning, 24 clinicians from 12 practices in the Virginia Ambulatory Care Outcomes Research Network (ACORN) and 87 intervention patients with uncontrolled chronic conditions participated in a care planning intervention. We had a structured process to guide patients, train navigators, and adapt the navigation process to meet the needs of each practice. Only 1 practice had bandwidth for staff to serve as a patient navigator, even for extra pay. For the other 11 practices, a research team member needed to provide navigation services. On average, patients wanted 25 weeks of support to complete care plans. The average time patients needed to speak with navigators on the phone was 7 min and 3 s. In exit interviews, patients consistently shared how motivational it was to have a caring person check in on them, offer help, and hold them accountable. Patient navigation to address care plans should be feasible. The time commitment is minimal. It does not require intensive training, and primary care is already doing much of this work. Yet, given the burden and competing demands in primary care, this help cannot be offered without additional resources.
Click the image to read our article in the Journal of Primary Care and Community Health.
Key themes
-

Care planning has a significant impact for patients.
In exit interviews, patients consistently shared how motivational it was to have a caring person check in on them, offer help, and hold them accountable.
-

Care planning is not time intensive.
On average, patients wanted 25 weeks of support to complete care plans.
Time commitment was minimal. The average time patients needed to speak with navigators on the phone was 7 minutes and 3 seconds.
Care planning does not require time intensive training.
-
Primary care needs additional resources to make care planning feasible.
Only 1 practice had bandwidth for staff to serve as a patient navigator, even for extra pay. For the other practices, a research team member needed to provide navigation services.
Primary care is already doing much of this work. Yet, given the burden and competing demands in primary care, this help cannot be offered without additional resources.
Patient
“[The patient navigator] asked me what else I could benefit from. And I told her that I desperately loved to have psychotherapy, if that was possible. And she says ‘I think I can arrange that.’ And the next thing I knew I was paired up with [a psychotherapist]. And we got the ball rolling and yeah, like life changing. Literally.”
Patient
“There was a time when I didn’t have a place to live. And I actually thought I was going to lose it because of the amount of responsibilities that was placed on me and [the patient navigator] was very instrumental and guided me to places that could offer me some assistance.”
Other publications and presentations
Click on any image below for full manuscript or file.
Patient Preferences for Discussing and Acting on Health-Related Needs in Primary Care, Journal of Primary Care and Community Health, August 2022
Exploring the Relationship Between Community Program Location and Community Needs, Journal of the American Board of Family Medicine, January 2022
Stakeholder input on a care planning tool to address unhealthy behaviors, mental health needs, and social risks: The value of different stakeholder perspectives, Journal of Clinical and Translational Science, October 2021
Enhanced care planning and clinical-community linkages versus usual care to address basic needs of patients with multiple chronic conditions: a clinician-level randomized controlled trial, Trials, June 2020
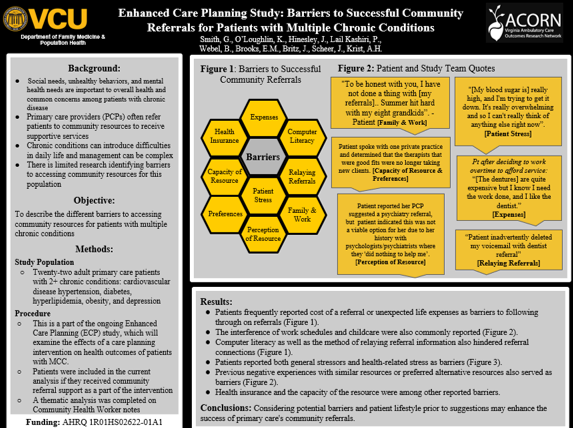
Enhanced Care Planning Study: Barriers to Successful Community Referrals for Patients with Multiple Chronic Conditions, 2021 North American Primary Care Research Group Conference (poster)
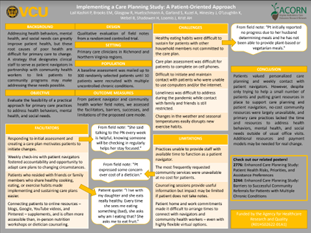
Implementing a Care Planning Study: A Patient-Oriented Approach, 2021 North American Primary Care Research Group Conference (poster)
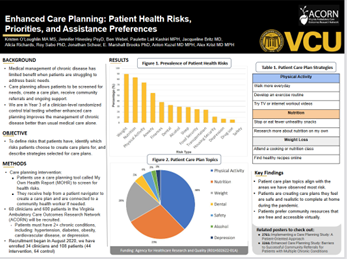
Enhanced Care Planning: Patient Health Risks, Priorities, and Assistance Preferences, 2021 North American Primary Care Research Group Conference (poster)
Stakeholder Input on an Enhanced Care Planning Tool Addressing Social Risk, Mental Health Needs, and Unhealthy Behaviors (poster)
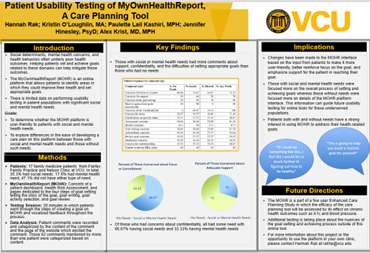
Patient Usability Testing of MyOwnHealthReport, A Care Planning Tool (poster)
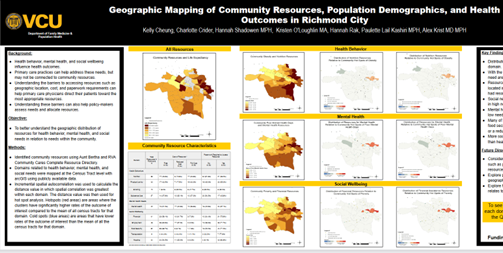
Geographic Mapping of Community Resources, Population Demographics, and Health Outcomes in Richmond City (poster)
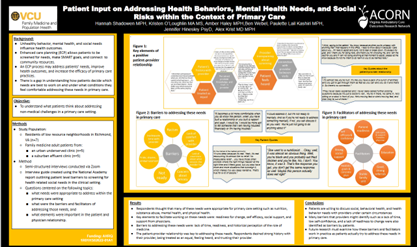
Patient Input on Addressing Health Behaviors, Mental Health Needs, and Social Risks within the Context of Primary Care (poster)
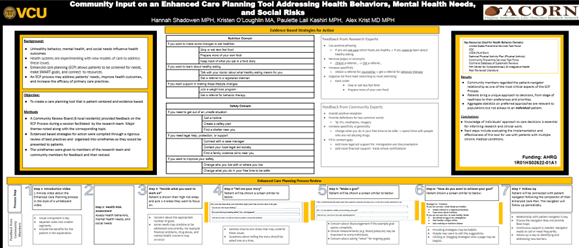
Community Input on an Enhanced Care Planning Tool Addressing Health Behaviors, Mental Health Needs, and Social Risks (poster)
Evaluating the Feasibility of Enhanced Care Planning for Primary Care Teams to Better Address Multiple Chronic Conditions, 2022 North American Primary Care Research Group Conference (presentation)
Evaluating the Feasibility of Enhanced Care Planning for Primary Care Teams to Better Address Multiple Chronic Conditions, 2022 Practice-Based Research Network Conference (presentation)
Enhanced Care Planning Study: Patient Prioritization of Needs and Assistance Preferences, 2021 Practice-Based Research Network Conference (presentation)
A Comparison of Needs Among Patients with Multiple Chronic Conditions and How Needs Impact Interest In Research Participation, 2021 Practice-Based Research Network Conference (presentation)